Taming the Heart: Beyond ACLS
Author: Adam Huynh MD
Peer Editors: Amy Hembree MD, Lauren Gruffi MD
Faculty Editor: Mary G. McGoldrick, MD
Introduction
Cardiac arrest, as defined by the American Heart Association (AHA), is the abrupt loss of heart function in a person who may or may not have been diagnosed with heart disease [1]. From the CARES (Cardiac Arrest Registry to Enhance Survival), approximately 356,000 cardiac arrests happen in the U.S. each year [2,3]. In 2024, 83.8% of adult out-of-hospital cardiac arrests were presumed to be of a cardiac cause with about 30% of arrests presenting with an initial shockable rhythm: ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT) [3]. The AHA Advanced Cardiac Life Support (ACLS) algorithm is an excellent framework to guide clinicians in the treatment and interventions for patients suffering from cardiac arrest. However, a certain subset of patients will remain in cardiac arrest with refractory VF and/or pVT despite ACLS interventions (ie. CPR, defibrillation, anti-arrhythmics).
To establish definitions, refractory VF/pVT is defined as an initial shockable rhythm that is still observed after three defibrillations, CPR, and standard ACLS medications (ie. amiodarone, epinephrine) [4]. Additionally, to emphasize, refractory VF/pVT is when the rhythm persists despite intervention; which is distinct from recurrent VF/pVT in which VF/pVT is converted to another rhythm but then returns [6]. Separately, Electrical Storm is defined as 3 or more sustained episodes of VF or pVT in 24 hours [5].
Although refractory VF is a small subset of patients in cardiac arrest, accounting for about 4% of patients who present initially with a shockable rhythm, the unique interventions in this patient population have been demonstrated to be lifesaving [4]. This article will discuss the evidence-based treatments for patients that require more than the standard ACLS resuscitation.
Dual Sequential External Defibrillation
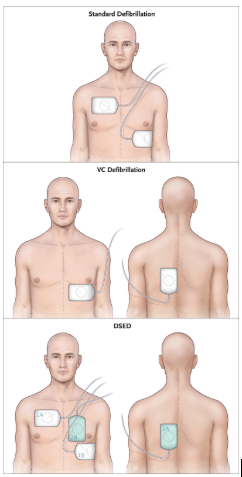
Double sequential external defibrillation (DSED) is rapid sequential shocks via two defibrillators with defibrillation pads placed in two planes (anterior-lateral and anterior–posterior) [7]. See the figure below.
Figure 1. Cheskes S, Verbeek PR, Drennan IR, et al. Defibrillation strategies for refractory ventricular fibrillation. N Engl J Med. 2022;387(21):1947–1956. doi: 10.1056/NEJMoa2207304
One of the most prominent pieces of evidence for DSED is the DOSE-VF trial.
The DOSE-VF trial was a prehospital study in Canada conducted in 2022. It was a cluster-randomized design evaluating strategies for refractory VF after three failed standard shocks in adult out-of-hospital cardiac arrest. Patients were assigned into 3 groups: standard defibrillation, vector-change defibrillation (switching defibrillation pads from anterior-lateral to an anterior-posterior position), or DSED using two defibrillators. Both alternative strategies improved outcomes, with DSED showing the highest survival to hospital discharge (~30%), followed by vector-change (~22%), compared with standard defibrillation (~13%). The trial demonstrated that changing defibrillation strategy significantly improves survival and neurologic outcomes in refractory VF [6,7].
More recently, a secondary analysis of DOSE-VF in 2024 divided patients into those with refractory VF and those with recurrent VF. They found that patients with recurrent VF had significantly better survival than those with refractory VF. Importantly, when standard defibrillation failed, DSED markedly improved survival and neurologic outcomes in both subgroups, whereas the vector-change strategy improved termination of VF but did not significantly improve survival or return of spontaneous circulation (ROSC) [8,9].
Esmolol
In the emergency department, esmolol is typically used in acute aortic pathology such as dissection. However, there is some evidence supporting its use for refractory VF/pVT.
The physiological rationale for using esmolol in refractory VF or pVT is based on breaking the cycle of catecholamine-driven electrical instability. During cardiac arrest, after multiple defibrillations, epinephrine doses, and CPR, the myocardium becomes highly adrenergically stimulated, increasing myocardial oxygen demand and arrhythmogenicity [10]. This heightened sympathetic tone makes VF/pVT more difficult to terminate and more likely to recur even after interventions. Esmolol, a short acting selective β1-blocker, temporarily blunts this adrenergic storm, which reduces myocardial excitability, and lowers oxygen consumption. Theoretically, by decreasing catecholamine-induced overstimulation, esmolol may make defibrillation more effective, reduce recurrent arrhythmia, and improve the likelihood of achieving and maintaining ROSC [10]. Typical dosing for esmolol in this setting would be 500mcg/kg IV bolus followed by a drip of a maximum of 100mcg/kg/min.
In 2023, a systematic review and meta-analysis studied esmolol use in the treatment of refractory VF and pVT. The authors identified two observational studies fitting their criteria of adult patients in refractory VF/pVT , totaling 66 patients, 22 of whom received esmolol. Their pooled analysis suggested that esmolol may improve rates of return of spontaneous circulation (RR 2.63 (95% CI 1.37–5.07), and survival to discharge (RR 2.82 (95% CI 1.01–7.93) [10]. It is important to note that the authors emphasize that the certainty of evidence is very low due to the small number of studies, methodological limitations, and high risk of bias.
Previously, a retrospective investigation in 2014 compared two groups of patients. One group who got standard ACLS care (n=19) and patients who got esmolol after standard ACLS (n=6). Of those 6 patients who received esmolol, 100% achieved ROSC. Although the actual number of patients was small, this investigation showed that the survival to discharge with a good neurologic outcome was 50% in the esmolol group compared to 11% in the control group [11].This highlights the need for prospective trials to define the true role of esmolol in refractory VF/pVT.
Stellate Ganglion Block
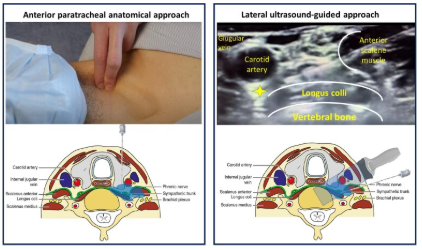
The stellate ganglion is part of the sympathetic nervous system located in the neck, and it provides sympathetic innervation to the heart. As stated above, in refractory ventricular arrhythmias, heightened sympathetic tone in cardiac arrest and subsequent interventions can worsen arrhythmias. A stellate ganglion block (SGB) involves injecting a local anesthetic under ultrasound-guidance to temporarily interrupt the sympathetic signals coming from the ganglion. By reducing sympathetic stimulation, SGB may reduce the burden of ventricular arrhythmias [13].
It is considered, however, a high risk procedure given the proximity of the ganglion to vulnerable structures. Details of this procedure are outside the scope of this article but be aware that the target area for the anesthetic is identified in the second photo of the sonogram with the yellow star (i.e. just posterior to the carotid artery).
Figure 2. Eur Heart J. 2024 Jan 30;45(10):823–833. doi: 10.1093/eurheartj/ehae021
The 2024 STAR study was a multicenter observational study evaluating stellate ganglion block for patients in a refractory ventricular arrhythmia/electrical storm who were failing standard antiarrhythmics and defibrillation. Among 131 patients who underwent 184 SGB procedures, 92% achieved the primary endpoint of at least a 50% reduction in VT/VF episodes in the 12 hours after the block, with the median number of arrhythmias dropping from 6 to 0. Major complications were rare, suggesting that SGB is an effective and safe adjunctive therapy for suppressing refractory VT/VF [12]. Although the results of the STAR study shows promise for the SGB, the generalizability of this study is difficult when extrapolating to the acute patient in the emergency department.
Beyond the STAR study, there are case series and reports showing effective termination of arrhythmias in patients with cardiac arrest [14, 15], but no large randomized controlled trial has been conducted thus far at the time of writing of this article.
ECMO
Extracorporeal membrane oxygenation (ECMO) is a mechanical circulatory support technique that temporarily takes over the function of the heart and lungs. In veno-arterial (VA) ECMO, blood is drained from a central vein, oxygenated and cleared of carbon dioxide in an external circuit, and then returned to a central artery, providing systemic perfusion and allowing vital organs to receive oxygenated blood even when the heart is in refractory VF/pVT [14]. ECMO is considered a bridge to other interventions such as coronary angiography and percutaneous coronary intervention. ECMO itself does not terminate arrhythmias, but it instead sustains circulation and organ perfusion, buying critical time for definitive therapies in what would otherwise be a fatal cardiac arrest [16].Extracorporeal CPR (eCPR) is defined as the rapid initiation of CPR in patients who experience a sudden or unexpected pulseless condition. [1]
One of the more notable publications on ECMO in refractory arrhythmia was the 2020 ARREST trial. This was a phase 2, single-center, randomized study comparing early ECMO‑facilitated resuscitation versus standard ACLS in adults in out-of-hospital cardiac arrest due to refractory VF or pVT after three failed shocks. Patients randomized to the ECMO arm were transported immediately upon hospital arrival to the cath lab, had veno-arterial ECMO initiated, and received coronary angiography if indicated. Of the 30 patients enrolled (15 in each arm, though 1 in the ECMO arm withdrew before discharge), 43% (6/14) of the ECMO group survived to hospital discharge versus 7% (1/15) in the standard ACLS group. The trial was stopped because of marked benefit in the ECMO group. This trial provides strong proof-of-concept that early eCPR can dramatically improve survival in otherwise fatal refractory VF, though it was small and at a single center [17].
In 2023, a larger follow-up study called the INCEPTION trial was published. This was a multicenter randomized controlled study in the Netherlands that compared eCPR versus standard CPR in 134 adults with refractory out-of-hospital cardiac arrest and an initial shockable rhythm. After 30 days, 20% of patients in the ECPR group survived with good neurologic outcome, versus 16% in the conventional CPR group, though this was a non-significant difference (OR 1.4; 95% CI, 0.5–3.5; P = 0.52). The authors concluded that in this trial context, early ECPR did not significantly improve neurologically favorable survival [18].
The ARREST (2020) and INCEPTION (2023) trials both evaluated early ECMO-facilitated resuscitation in refractory out-of-hospital cardiac arrest, but they differed in scale and outcomes. ARREST provided proof-of-concept that early ECMO can dramatically improve survival in refractory VF, while INCEPTION suggests that, in broader multicenter practice, the benefit is smaller and less certain, highlighting the importance of patient selection, logistics, and center experience.
Takeaway
Refractory VF and pulseless VT occur in a small but critically important subset of cardiac arrest patients who do not respond to standard ACLS interventions. Emerging therapies including dual sequential external defibrillation, esmolol, stellate ganglion block, and ECMO should be employed in an evidence-based manner to treat this critical group of patients. Evidence suggests:
DSED improves survival and neurologic outcomes after failed standard shocks
Esmolol may blunt adrenergic storm to facilitate defibrillation
SGB can significantly reduce arrhythmia burden
ECMO provides circulatory support to bridge patients to other advanced therapies
Overall, these interventions highlight the importance of a comprehensive, multimodal approach for refractory VF/pVT, combining advanced pharmacologic, procedural, and mechanical strategies to improve survival in this high-risk population.
References
1. “What Is Cardiac Arrest?” Www.Heart.Org, https://www.heart.org/en/health-topics/cardiac-arrest/about-cardiac-arrest. Accessed 17 Nov. 2025.
2. Tsao, Connie W., et al. “Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association.” Circulation, vol. 145, no. 8, Feb. 2022, pp. e153–639. PubMed, https://doi.org/10.1161/CIR.0000000000001052.
3. 2024 CARES Annual Report. https://mycares.net/sitepages/uploads/2025/2024_flipbook/index.html?page=1. Accessed 17 Nov. 2025.
4. Verkaik, Bas J, et al. “Abstract 419: Incidence of True Refractory Ventricular Fibrillation in Patients Meeting a Pragmatic Definition of Refractory Ventricular Fibrillation.” Circulation, vol. 148, no. Suppl_1, Nov. 2023. DOI.org (Crossref), https://doi.org/10.1161/circ.148.suppl_1.419.
5. Eifling, Michael, et al. “The Evaluation and Management of Electrical Storm.” Texas Heart Institute Journal, vol. 38, no. 2, 2011, pp. 111–21. PubMed Central, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3066819/.
6. Toomey, David. “Updates in the Management of Refractory Ventricular Tachycardia or Ventricular Fibrillation Arrest.” ACEP Now, https://www.acepnow.com/article/updates-in-the-management-of-refractory-ventricular-tachycardia-or-ventricular-fibrillation-arrest/. Accessed 17 Nov. 2025.
7. Cheskes, Sheldon, et al. “Double Sequential External Defibrillation for Refractory Ventricular Fibrillation.” Intensive Care Medicine, vol. 49, no. 4, 2023, pp. 455–57. PubMed Central, https://doi.org/10.1007/s00134-023-06993-1.
8. Cheskes, Sheldon, et al. “Defibrillation Strategies for Refractory Ventricular Fibrillation.” New England Journal of Medicine, vol. 387, no. 21, Nov. 2022, pp. 1947–56. DOI.org (Crossref), https://doi.org/10.1056/NEJMoa2207304.
9. Cheskes, Sheldon, et al. “The Impact of Alternate Defibrillation Strategies on Shock-Refractory and Recurrent Ventricular Fibrillation: A Secondary Analysis of the DOSE VF Cluster Randomized Controlled Trial.” Resuscitation, vol. 198, May 2024, p. 110186. PubMed, https://doi.org/10.1016/j.resuscitation.2024.110186.
10. Hesegawa, Daisuke, et al. “A SYSTEMATIC REVIEW AND META-ANALYSIS OF ESMOLOL FOR REFRACTORY VENTRICULAR FIBRILLATION AND PULSELESS VENTRICULAR TACHYCARDIA” Chest, vol. 164, October 2023
11. Driver, Brian E., et al. “Use of Esmolol after Failure of Standard Cardiopulmonary Resuscitation to Treat Patients with Refractory Ventricular Fibrillation.” Resuscitation, vol. 85, no. 10, Oct. 2014, pp. 1337–41. PubMed, https://doi.org/10.1016/j.resuscitation.2014.06.032.
12. Savastano, Simone, et al. “Electrical Storm Treatment by Percutaneous Stellate Ganglion Block: The STAR Study.” European Heart Journal, vol. 45, no. 10, Mar. 2024, pp. 823–33. PubMed, https://doi.org/10.1093/eurheartj/ehae021.
13. Piraccini, Emanuele, et al. “Stellate Ganglion Blocks.” StatPearls, StatPearls Publishing, 2025. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK507798/.
14. Banerjee A, Mishra A, Batra A, Vatsa D, Chauhan P. A Case Report on USG-Guided Stellate Ganglion Block in Refractory Ventricular Tachycardia. J Pharm Bioallied Sci. 2025 Jun;17(Suppl 2):S2001-S2003. doi: 10.4103/jpbs.jpbs_174_25. Epub 2025 Jun 18. PMID: 40655668; PMCID: PMC12244658.
15. Fudim M, Qadri YJ, Waldron NH, Boortz-Marx RL, Ganesh A, Patel CB, Podgoreanu MV, Sun AY, Milano CA, Tong BC, Harpole DH Jr, Mathew JP, Piccini JP. Stellate Ganglion Blockade for the Treatment of Refractory Ventricular Arrhythmias. JACC Clin Electrophysiol. 2020 May;6(5):562-571. doi:
16. Vyas, Ankit, et al. “Extracorporeal Membrane Oxygenation in Adults.” StatPearls, StatPearls Publishing, 2025. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK576426/.
17. Baran DA. Extracorporeal Membrane Oxygenation (ECMO) and the Critical Cardiac Patient. Curr Transplant Rep. 2017;4(3):218-225. doi: 10.1007/s40472-017-0158-5. Epub 2017 Jul 10. PMID: 28932651; PMCID: PMC5577059.
1016/j.jacep.2019.12.017. Epub 2020 Feb 26. PMID: 32439042.
18. Kumar KM. ECPR-extracorporeal cardiopulmonary resuscitation. Indian J Thorac Cardiovasc Surg. 2021 Apr;37(Suppl 2):294-302. doi: 10.1007/s12055-020-01072-2. Epub 2021 Jan 7. PMID: 33432257; PMCID: PMC7787697.
19. Yannopolis, Demtris, et al. “Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial” The Lancet, vol 396, December 2020
20. Suverein, Martje M., et al. “Early Extracorporeal CPR for Refractory Out-of-Hospital Cardiac Arrest.” New England Journal of Medicine, vol. 388, no. 4, Jan. 2023, pp. 299–309. DOI.org (Crossref), https://doi.org/10.1056/NEJMoa2204511